Osteomyelitis: A Comprehensive Guide to Bone Infection
Osteomyelitis is a serious medical condition characterized by inflammation and infection of the bone, typically caused by bacteria. In some cases, fungi can also be responsible for the infection. This condition can affect people of all ages, though certain risk factors make some individuals more susceptible. Without prompt and effective treatment, osteomyelitis can lead to severe complications, including the destruction of bone tissue, permanent disability, and even death.
This article provides a detailed look at the causes, symptoms, diagnosis, and treatment options for osteomyelitis. Understanding this condition is crucial for recognizing early signs and seeking appropriate medical care to prevent long-term consequences.
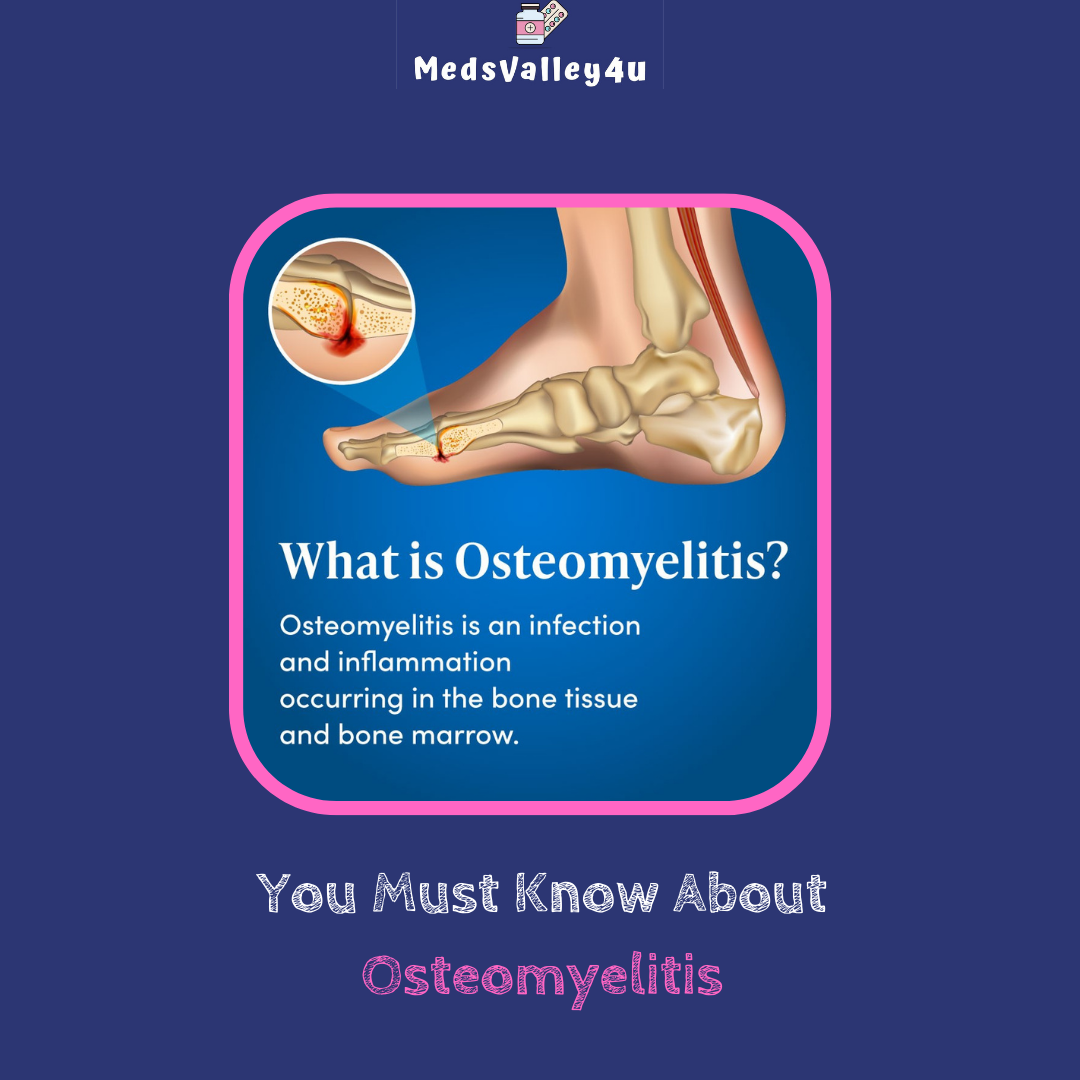
What is Osteomyelitis?
Osteomyelitis is an infection that reaches a bone, either through the bloodstream, direct injury, or nearby tissue infection. The infection can spread quickly and result in inflammation, which impedes blood circulation in the bone. Over time, the affected bone can deteriorate, and without adequate blood flow, parts of the bone may die (necrosis).
There are two primary types of osteomyelitis:
- Acute Osteomyelitis: This form of the disease develops quickly and is most common in children. It can often be treated successfully with antibiotics, especially when diagnosed early.
- Chronic Osteomyelitis: If the infection persists or recurs over time, it becomes chronic. Chronic osteomyelitis may result from an inadequately treated acute infection or an ongoing health issue like diabetes or a weak immune system.
Causes of Osteomyelitis
Osteomyelitis can be caused by several different factors, most commonly by bacteria entering the bone. The bacterium Staphylococcus aureus is the most frequent culprit. Below are the common causes and routes by which the infection reaches the bone:
1. Bloodstream Infections:
Bacteria that enter the bloodstream through another infection in the body (such as pneumonia, a urinary tract infection, or skin infections) can travel to the bone. This is known as hematogenous osteomyelitis. It is more common in children because their bones are still developing and have a rich blood supply, making them more susceptible to infection.
2. Open Fractures or Bone Surgery:
When a bone is exposed due to a fracture or surgical procedure, it becomes vulnerable to infection. This form of osteomyelitis is known as direct inoculation osteomyelitis. Orthopedic surgeries, especially those involving the placement of metal hardware like screws, plates, or prosthetics, can introduce bacteria to the bone.
3. Infection from Nearby Tissue:
Infections in nearby tissues, such as muscles, skin, or tendons, can spread to the bones, particularly in individuals with compromised immune systems. This condition is known as contiguous osteomyelitis. Diabetics are particularly vulnerable to this type because of poor wound healing, especially in the feet.
4. Poor Circulation:
Conditions that impair blood flow, such as diabetes, atherosclerosis, or smoking, can reduce the body’s ability to fight infections. When blood supply to the bone is compromised, the risk of osteomyelitis increases.
5. Immune System Weakness:
Individuals with weakened immune systems—whether due to chronic conditions, HIV/AIDS, cancer treatments, or immunosuppressive medications—are at a higher risk for developing infections, including osteomyelitis.
Symptoms of Osteomyelitis
The symptoms of osteomyelitis can vary depending on whether the infection is acute or chronic, the affected bone, and the person’s overall health. Common symptoms include:
1. Pain and Tenderness:
One of the earliest and most common symptoms of osteomyelitis is pain in the affected bone. This pain may be persistent, worsen with movement, and feel deep or throbbing. The area may also become tender to touch.
2. Swelling, Warmth, and Redness:
The infected area often becomes swollen, red, and warm as the body tries to fight off the infection. This is particularly noticeable if the infection is near the surface of the skin.
3. Fever and Chills:
In acute cases, fever and chills may develop as the body responds to the infection. In children, this can be one of the first signs of osteomyelitis, accompanied by lethargy or irritability.
4. Limited Range of Motion:
Infected bones in the limbs can lead to difficulty moving joints near the infection. This can cause stiffness or reduced mobility, especially if the infection is in the spine or joints.
5. Drainage of Pus:
In chronic osteomyelitis, pus may drain from the infected area if the infection breaks through the skin. This is a sign of severe infection and tissue damage.
6. Fatigue or Malaise:
A general feeling of weakness or tiredness may accompany osteomyelitis, as the body’s immune system fights the infection.
Risk Factors for Osteomyelitis
Certain factors increase the risk of developing osteomyelitis, including:
- Diabetes: Poor blood circulation, nerve damage, and a weakened immune system make diabetics more susceptible to infections, particularly in the feet.
- Recent Injury or Surgery: Any surgical procedure involving bones or joints, as well as open wounds from injuries, can introduce bacteria to the bone.
- Chronic Illnesses: Conditions that weaken the immune system, such as cancer, kidney failure, or HIV, increase the risk of infections.
- Intravenous Drug Use: People who use intravenous drugs may introduce bacteria directly into the bloodstream, increasing the risk of bloodstream infections and subsequent osteomyelitis.
- Peripheral Artery Disease (PAD): Reduced blood flow in the limbs due to PAD can increase the likelihood of bone infections.
- Prosthetic Implants: Artificial joints or bone hardware can harbor bacteria, increasing the risk of osteomyelitis, particularly if the hardware becomes infected.
Diagnosing Osteomyelitis
Osteomyelitis can be difficult to diagnose because its symptoms often mimic other conditions. However, early and accurate diagnosis is crucial for effective treatment. Diagnosis typically involves a combination of the following tests:
1. Blood Tests:
Blood tests can reveal signs of infection, such as elevated white blood cell counts and increased levels of inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). However, blood tests alone cannot confirm osteomyelitis.
2. Imaging Studies:
- X-rays: Though X-rays may not detect early stages of infection, they can reveal bone damage in chronic cases.
- MRI (Magnetic Resonance Imaging): MRI scans are more sensitive than X-rays and can detect infections in soft tissues and bones earlier.
- CT Scans (Computed Tomography): CT scans provide detailed images of bones and can help in detecting bone infections.
- Bone Scans: A bone scan can identify areas of increased bone activity, indicating infection or inflammation.
3. Bone Biopsy:
The most definitive test for diagnosing osteomyelitis is a bone biopsy. A sample of bone tissue is taken and tested to determine the specific type of bacteria or fungi causing the infection. This information is crucial for selecting the most effective antibiotic or antifungal treatment.
Treatment of Osteomyelitis
Treatment for osteomyelitis typically involves a combination of antibiotics, surgery, and supportive care. The specific treatment plan depends on the severity of the infection, the type of bacteria or fungus involved, and the patient’s overall health.
1. Antibiotic Therapy:
Intravenous (IV) antibiotics are the mainstay of treatment for bacterial osteomyelitis. The choice of antibiotic depends on the specific bacteria identified from the bone biopsy. IV antibiotics are usually given for several weeks, followed by oral antibiotics for some time. For less severe cases, oral antibiotics may be sufficient.
2. Surgical Treatment:
In some cases, surgery is required to remove infected bone tissue, drain abscesses, or remove any foreign objects, such as metal hardware, that may be causing or exacerbating the infection. Surgery may involve:
- Debridement: Removal of dead or infected bone and tissue.
- Bone Grafting: In cases of extensive bone loss, a bone graft may be necessary to promote healing and restore bone integrity.
- Amputation: In severe, life-threatening cases, where the infection cannot be controlled, amputation may be necessary to prevent the spread of the infection.
3. Supportive Care:
Proper wound care, nutrition, and physical therapy can aid in the recovery process. In patients with chronic osteomyelitis, long-term monitoring and management are essential to prevent recurrent infections.
Preventing Osteomyelitis
Preventing osteomyelitis involves minimizing the risk of infection, particularly in individuals with known risk factors:
- Manage Chronic Conditions: For people with diabetes or vascular disease, managing blood sugar levels and improving circulation is essential for preventing infections.
- Proper Wound Care: Cleaning and covering wounds, especially after surgery or injury, can prevent bacteria from entering the body.
- Healthy Lifestyle Choices: Quitting smoking, maintaining a balanced diet, and avoiding intravenous drug use can reduce the risk of osteomyelitis.
Conclusion
Osteomyelitis is a serious condition that requires prompt diagnosis and treatment to prevent long-term damage to bones and surrounding tissues. While it can be a challenging condition to treat, advances in medical imaging, antibiotics, and surgical techniques have improved the outcomes for many patients. Early intervention, appropriate use of antibiotics, and preventive measures are key to managing osteomyelitis effectively and minimizing the risk of complications.




Write a comment
Your email address will not be published. All fields are required