Diabetic Neuropathy: Explanation and Treatment Options
Diabetic neuropathy is a type of nerve damage that can occur in individuals with diabetes, particularly when blood sugar levels are poorly controlled over time. This condition can affect various nerves throughout the body, leading to a range of symptoms, from pain and numbness to digestive and cardiovascular issues. Understanding diabetic neuropathy, its types, symptoms, causes, and treatment options, is crucial for effective management and prevention of complications.
What is Diabetic Neuropathy?
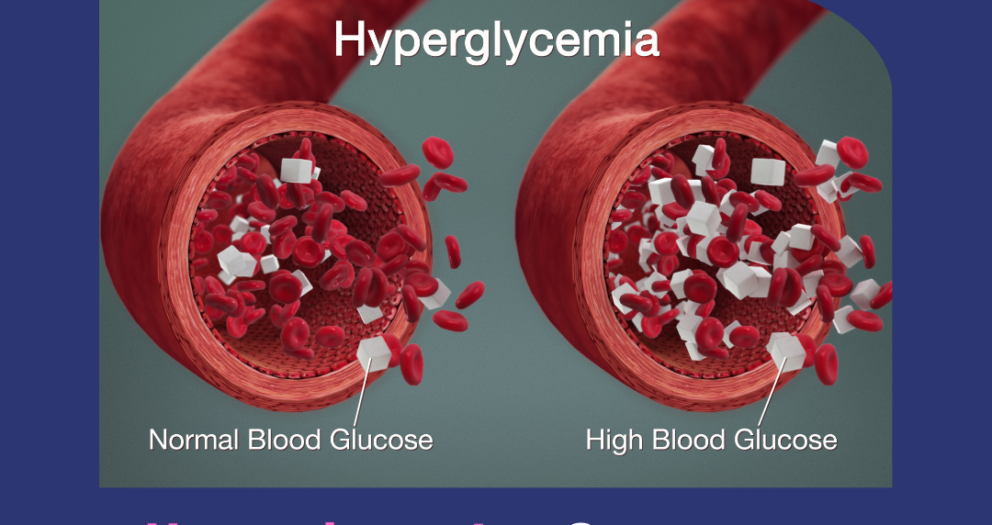
Diabetic neuropathy is one of the most common complications of diabetes, affecting about 50% of people with the condition. It occurs when prolonged high blood glucose levels damage the nerves, which are responsible for transmitting signals between the brain and other parts of the body. This nerve damage impairs the body’s ability to function properly and can manifest in various ways, depending on which nerves are affected.
Nerves in the legs and feet are most often affected, but diabetic neuropathy can also impact nerves in other areas, including the digestive system, heart, and bladder. In severe cases, it can lead to significant disability, affecting an individual’s quality of life.
Types of Diabetic Neuropathy
There are four main types of diabetic neuropathy, each with its own set of symptoms and affected areas:
- Peripheral Neuropathy:
This is the most common type of diabetic neuropathy and primarily affects the feet, legs, hands, and arms. It typically causes pain, tingling, numbness, and a burning sensation in these areas. In severe cases, it can lead to muscle weakness, balance issues, and an increased risk of foot injuries or ulcers. - Autonomic Neuropathy:
Autonomic neuropathy affects the autonomic nervous system, which controls involuntary bodily functions, such as heart rate, digestion, and bladder control. It can lead to a variety of issues, including difficulty swallowing, digestive problems, abnormal sweating, and issues with sexual function. In extreme cases, it can also result in sudden drops in blood pressure (orthostatic hypotension) or irregular heartbeats (arrhythmia). - Proximal Neuropathy (Diabetic Amyotrophy):
This form of neuropathy affects the nerves in the hips, thighs, buttocks, or legs. It can cause sudden, severe pain, weakness in the legs, and muscle wasting. Unlike peripheral neuropathy, proximal neuropathy often improves over time, but it can take months or even years for full recovery. - Focal Neuropathy (Mononeuropathy):
Focal neuropathy affects a specific nerve, usually in the head, torso, or leg. It often occurs suddenly and can cause severe pain or weakness in one part of the body, such as the eye, face, or leg. While focal neuropathy can be alarming, it usually improves over weeks or months.
Symptoms of Diabetic Neuropathy
The symptoms of diabetic neuropathy can vary depending on the type and the specific nerves affected. Common symptoms include:
- Peripheral Neuropathy Symptoms:
- Tingling or burning sensations, especially in the feet and legs
- Numbness or reduced ability to feel pain or temperature changes
- Sharp pains or cramps
- Increased sensitivity to touch
- Muscle weakness
- Loss of coordination and balance
- Foot ulcers, infections, or joint pain due to unnoticed injuries
- Autonomic Neuropathy Symptoms:
- Bladder problems, such as difficulty emptying the bladder completely
- Bloating, nausea, or vomiting, especially after meals
- Constipation or diarrhea, particularly at night
- Difficulty swallowing
- Abnormal sweating, either too much or too little
- Sexual dysfunction, including erectile dysfunction in men and vaginal dryness in women
- Heart rate or blood pressure irregularities, such as dizziness upon standing
-
Proximal Neuropathy Symptoms:
- Sudden, severe pain in the hip, thigh, or buttock
- Weakness in the legs
- Difficulty rising from a seated position
- Unexplained weight loss
-
Focal Neuropathy Symptoms:
- Pain in the chest, abdomen, or lower back
- Eye problems, including double vision or difficulty focusing
- Paralysis on one side of the face (Bell’s palsy)
- Pain in specific areas, such as the front of the thigh or foot
Causes of Diabetic Neuropathy
The primary cause of diabetic neuropathy is prolonged exposure to high blood sugar levels. Over time, elevated glucose damages the blood vessels that supply the nerves, which leads to reduced nutrient delivery and nerve damage. Other factors that may contribute to the development of diabetic neuropathy include:
- High Blood Pressure: Hypertension can damage the blood vessels that supply nerves, worsening the impact of high blood sugar.
- High Cholesterol: Excess cholesterol can contribute to plaque buildup in the arteries, reducing blood flow to the nerves.
- Smoking: Smoking constricts blood vessels, reducing circulation to the nerves and exacerbating nerve damage.
- Genetics: Some people may be genetically predisposed to nerve damage, making them more susceptible to developing neuropathy.
- Age: The risk of developing diabetic neuropathy increases with age, especially for individuals with long-standing diabetes.
How is Diabetic Neuropathy Treated?
There is no cure for diabetic neuropathy, but there are treatments available to manage symptoms, slow the progression of the disease, and improve the quality of life. The treatment plan for diabetic neuropathy typically includes a combination of lifestyle changes, medications, and other interventions aimed at controlling blood sugar levels, relieving pain, and preventing complications.
1. Blood Sugar Control
The most critical aspect of treating diabetic neuropathy is maintaining optimal blood sugar levels. By keeping blood glucose within the target range, individuals can prevent further nerve damage and slow the progression of neuropathy. Strategies for controlling blood sugar include:
- Diet: Following a balanced, low-carbohydrate diet can help regulate blood sugar levels. Focus on whole grains, lean proteins, healthy fats, and plenty of vegetables.
- Exercise: Regular physical activity improves insulin sensitivity, enhances circulation, and helps regulate blood sugar levels.
- Medications: Individuals with diabetes may need oral medications or insulin therapy to control their blood sugar effectively.
2. Medications for Pain Relief
Many individuals with diabetic neuropathy experience chronic pain, which can significantly affect their quality of life. Several types of medications are commonly used to manage neuropathic pain, including:
- Over-the-Counter Pain Relievers: Mild pain can sometimes be managed with over-the-counter options like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.
- Antidepressants: Certain antidepressants, such as amitriptyline, duloxetine, and nortriptyline, are effective in treating neuropathic pain by interfering with pain signals in the brain.
- Anticonvulsants: Medications typically used to treat seizures, such as pregabalin and gabapentin, are also effective for reducing nerve pain.
- Topical Treatments: Capsaicin cream and lidocaine patches can be applied to the skin to provide localized pain relief.
- Opioids: In cases of severe pain that doesn’t respond to other treatments, opioids may be prescribed. However, due to their risk of addiction and side effects, they are usually considered a last resort.
3. Lifestyle Modifications
In addition to controlling blood sugar, several lifestyle modifications can help manage diabetic neuropathy and reduce the risk of complications:
- Foot Care: Proper foot care is essential for individuals with diabetic peripheral neuropathy. Regularly inspect the feet for cuts, blisters, or sores, as neuropathy may reduce sensation, making injuries harder to detect. Wearing well-fitting shoes and keeping the feet clean and moisturized can prevent infections and ulcers.
- Smoking Cessation: Quitting smoking improves circulation and reduces the risk of further nerve damage.
- Diet and Weight Management: Maintaining a healthy diet and body weight can reduce stress on the nerves and improve overall health.
- Stress Management: Practices such as yoga, meditation, and deep breathing can help reduce stress, which may exacerbate symptoms of diabetic neuropathy.
4. Physical Therapy
For individuals with muscle weakness or mobility issues caused by neuropathy, physical therapy can be beneficial. A physical therapist can design a personalized exercise program to improve strength, balance, and coordination, helping to prevent falls and other injuries.
5. Surgical Options
In rare cases, individuals with severe focal neuropathy may require surgery to relieve pressure on a nerve (e.g., carpal tunnel syndrome) or address other structural issues causing nerve damage.
Conclusion
Diabetic neuropathy is a serious complication of diabetes that can significantly impact an individual’s quality of life. While there is no cure, managing blood sugar levels, relieving pain, and making lifestyle changes can help control symptoms and slow the progression of the disease. With proper care and treatment, individuals with diabetic neuropathy can minimize complications and maintain a better quality of life. Early diagnosis and intervention are crucial to preventing severe damage and reducing the risk of further nerve deterioration.

Write a comment
Your email address will not be published. All fields are required