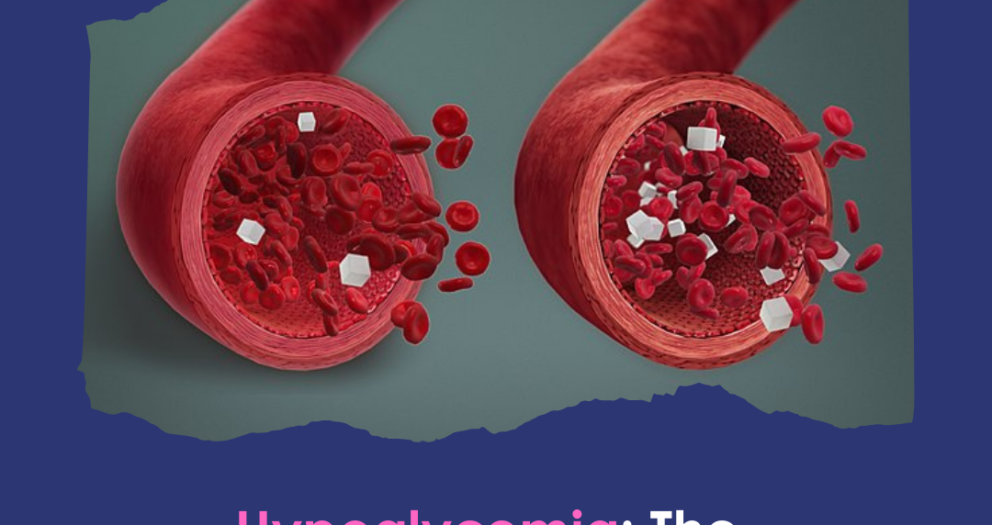
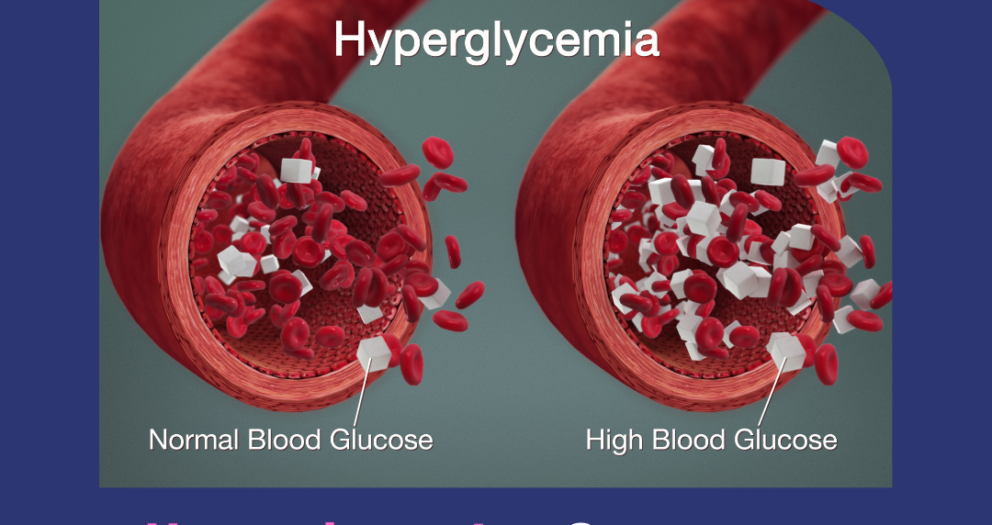
Hypoglycemia: The Condition of Having Blood Sugar Levels Too Low.
Hypoglycemia is a medical condition characterized by abnormally low blood sugar (glucose) levels, typically below 70 mg/dL. Glucose is the body’s primary source of energy, especially for the brain and nervous system. When blood sugar drops too low, the body cannot function optimally, leading to a range of symptoms that can be mild, moderate, or severe. In extreme cases, hypoglycemia can be life-threatening if not treated promptly.
While hypoglycemia is most commonly associated with diabetes and the use of insulin or oral hypoglycemic medications, it can also occur in individuals without diabetes due to other medical conditions, dietary habits, or lifestyle factors. Understanding the causes, symptoms, and treatments for hypoglycemia is crucial for managing the condition and preventing complications.
What is Hypoglycemia?
Hypoglycemia occurs when the body’s glucose levels fall below a certain threshold. Glucose is a sugar that comes from food, particularly carbohydrates and is essential for energy production. After you eat, your body breaks down carbohydrates into glucose, which enters the bloodstream. Insulin, a hormone produced by the pancreas, helps cells absorb glucose and use it for energy. In healthy individuals, blood sugar levels are regulated within a narrow range by hormones like insulin and glucagon. However, in people with hypoglycemia, this balance is disrupted, and blood sugar levels drop below normal. The symptoms of hypoglycemia can vary depending on how low the blood sugar levels are, how quickly they fall, and how long they stay low.Symptoms of Hypoglycemia
The symptoms of hypoglycemia are the body's response to a lack of glucose, which is needed for energy and normal brain function. These symptoms can be categorized into early signs and more severe signs.Early Symptoms (Mild Hypoglycemia):
- Shakiness or Trembling: Low blood sugar triggers the release of adrenaline, which can cause tremors or shakiness in the hands and body.
- Sweating: Excessive sweating is another common sign of hypoglycemia, especially during periods of low activity or rest.
- Hunger: A sudden and intense feeling of hunger is a signal that the body is craving glucose for energy.
- Dizziness or Lightheadedness: As blood sugar drops, the brain may struggle to function properly, leading to dizziness or difficulty concentrating.
- Palpitations or Rapid Heart Rate: Hypoglycemia often leads to an increased heart rate as the body reacts to low blood sugar levels.
- Anxiety or Nervousness: Low blood sugar can make a person feel jittery, anxious, or on edge.
- Nausea: A sensation of nausea may occur, especially if the individual hasn’t eaten for an extended period.
Moderate to Severe Symptoms (Severe Hypoglycemia):
- Confusion or Disorientation: The brain depends on glucose for proper functioning. Severe hypoglycemia can impair cognitive abilities, making it difficult to think clearly or make decisions.
- Difficulty Speaking or Slurred Speech: As blood sugar drops, speech may become slow, slurred, or incoherent.
- Blurred Vision: Low blood sugar can affect the eyes, causing blurred vision or even double vision.
- Weakness or Fatigue: Without enough glucose for energy, muscles, and nerves may feel weak or fatigued.
- Seizures or Convulsions: In extreme cases, hypoglycemia can lead to seizures due to the brain’s lack of glucose.
- Loss of Consciousness (Coma): Prolonged or severe hypoglycemia can cause fainting or coma if not treated immediately.
Causes of Hypoglycemia
Hypoglycemia is most commonly seen in people with diabetes who take insulin or other blood sugar-lowering medications. However, it can also occur in individuals without diabetes. The following are common causes of hypoglycemia:1. Diabetes and Diabetes Medications:
- Insulin Use: People with diabetes who use insulin injections to manage their blood sugar are at risk of hypoglycemia if they take too much insulin relative to their food intake or physical activity level.
- Oral Medications: Certain diabetes medications, such as sulfonylureas (e.g., glipizide, glyburide) and meglitinides, can lower blood sugar too much, especially if meals are skipped or delayed.
2. Skipping or Delaying Meals:
- Prolonged Fasting: Skipping meals or going too long without eating can cause blood sugar to drop, particularly in individuals taking diabetes medications.
- Unbalanced Meals: Consuming meals that lack carbohydrates, or eating meals high in sugar without enough protein and fat, can cause rapid spikes and subsequent drops in blood sugar levels.
3. Intense Physical Activity:
- Exercise: Physical activity increases the body’s need for glucose, and without enough food or carbohydrate intake, exercise can deplete blood sugar levels and lead to hypoglycemia.
4. Alcohol Consumption:
- Alcohol-Induced Hypoglycemia: Drinking alcohol, especially on an empty stomach, can block the liver from releasing glucose into the bloodstream, leading to hypoglycemia. This is particularly dangerous for people with diabetes.
5. Hormonal Imbalances:
- Adrenal or Pituitary Disorders: The adrenal and pituitary glands regulate hormones involved in glucose production and storage. Conditions like Addison’s disease or growth hormone deficiencies can lead to hypoglycemia.
6. Critical Illnesses:
- Liver Disease: The liver plays a key role in glucose storage and release. In people with liver diseases such as hepatitis or cirrhosis, glucose production may be impaired, leading to hypoglycemia.
- Kidney Disease: The kidneys help to metabolize insulin, and in advanced kidney disease, insulin levels may become too high, leading to low blood sugar.
7. Insulinoma:
- Pancreatic Tumors: Rare tumors of the pancreas called insulinomas can produce excessive amounts of insulin, leading to chronic hypoglycemia in non-diabetic individuals.
Risk Factors for Hypoglycemia
Several factors can increase the risk of hypoglycemia. These include:- Taking Diabetes Medications: People with diabetes who take insulin or certain oral medications are at greater risk.
- Frequent Exercise: Intense or prolonged exercise can deplete blood sugar, especially if carbohydrates are not consumed beforehand.
- Alcohol Consumption: Drinking alcohol, particularly in large amounts or without food, can block glucose production in the liver.
- Skipping Meals: Irregular eating patterns or fasting increases the risk of hypoglycemia.
- Certain Health Conditions: Individuals with liver disease, kidney disease, adrenal insufficiency, or tumors like insulinomas are at higher risk.
Diagnosing Hypoglycemia
Hypoglycemia is diagnosed through blood tests that measure glucose levels. A diagnosis typically requires:- Blood Glucose Test: A blood glucose level below 70 mg/dL is generally considered hypoglycemic, though the threshold may vary depending on individual circumstances.
- Whipple’s Triad: To confirm the diagnosis, physicians often look for Whipple’s Triad, which includes low blood sugar levels, symptoms of hypoglycemia, and relief of those symptoms after blood sugar is raised.
Treatment of Hypoglycemia
The treatment of hypoglycemia depends on the severity of symptoms and the underlying cause. The goal is to quickly restore normal blood sugar levels and prevent recurrence.1. Immediate Treatment for Mild Hypoglycemia:
- Consuming Fast-Acting Carbohydrates: The first step is to raise blood sugar by consuming 15-20 grams of fast-acting carbohydrates, such as:
- Glucose tablets or gel.
- A small glass of fruit juice.
- Regular soda (not diet).
- Hard candies or sugar.
- After 15 minutes, blood sugar should be rechecked. If it’s still low, another 15 grams of carbohydrates should be consumed.
2. Treatment for Severe Hypoglycemia:
- Glucagon Injection: For severe cases where the individual is unconscious or unable to swallow, an injection of glucagon, a hormone that stimulates the liver to release glucose, is required.
- Emergency Medical Care: If glucagon is not available, or if the person does not respond to treatment, emergency medical help should be sought immediately.
3. Long-Term Management:
- Adjusting Medications: In people with diabetes, insulin or oral medication doses may need to be adjusted to prevent future episodes of hypoglycemia.
- Dietary Changes: Eating regular meals and snacks that contain carbohydrates, protein, and healthy fats can help stabilize blood sugar levels.
- Exercise Planning: People at risk for hypoglycemia should plan their physical activities and ensure they consume enough carbohydrates before and after exercise.
- Alcohol Moderation: Limiting alcohol intake and never drinking on an empty stomach can help prevent alcohol-induced hypoglycemia.
Preventing Hypoglycemia
Preventing hypoglycemia involves careful planning, especially for individuals with diabetes or other underlying conditions. Strategies include:- Monitoring Blood Sugar: Regularly checking blood sugar levels, especially before and after meals and exercise, can help prevent drops in glucose.
- Eating Balanced Meals: Consuming meals that contain a balance of carbohydrates, proteins, and fats helps maintain steady blood sugar levels.
- Carrying Fast-Acting Carbs: Keeping glucose tablets, candy, or juice on hand ensures quick treatment if symptoms of hypoglycemia arise.
- Following Medical Advice: Adjusting diabetes medications and insulin dosages based on lifestyle factors, such as exercise and diet, can help reduce the risk of hypoglycemia.